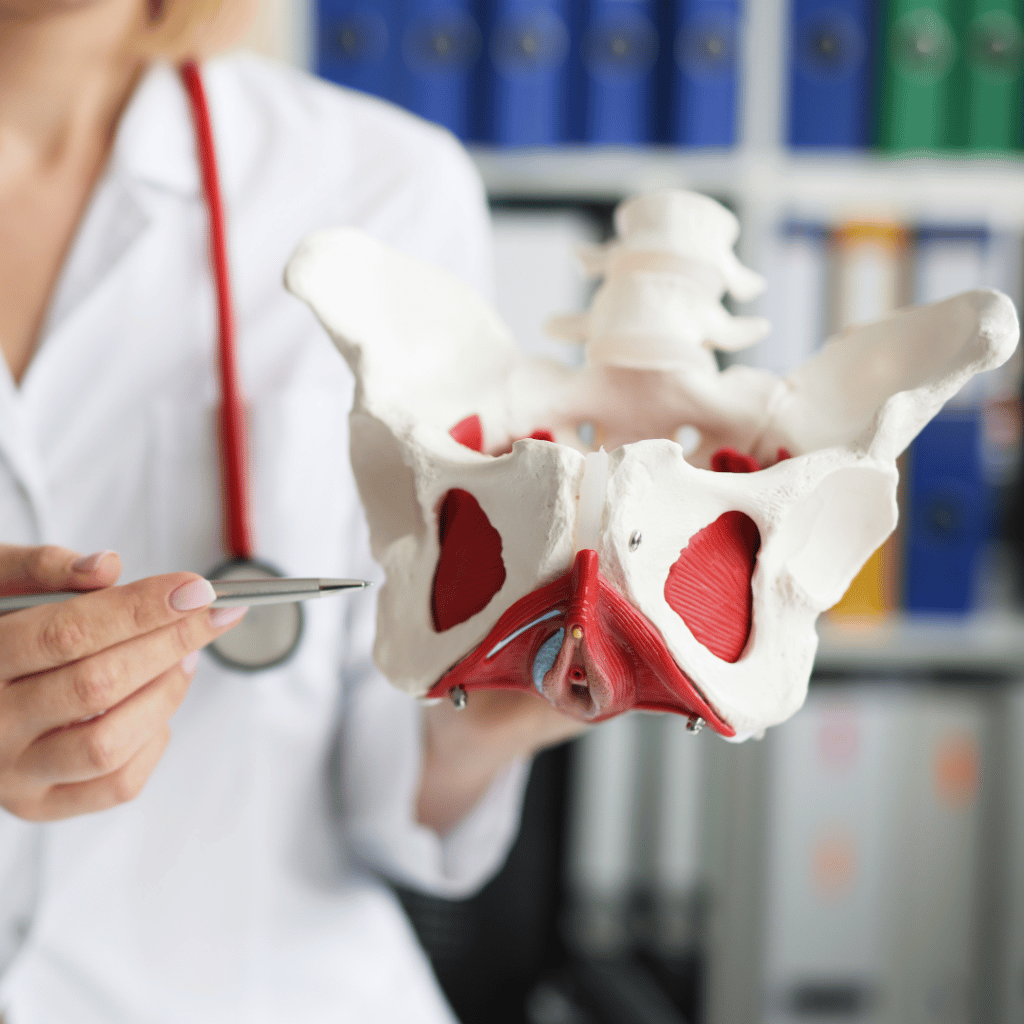
Pelvic Muscle Rehabilitation: Supporting Patients with Pelvic Floor Dysfunction
Patients with pelvic floor dysfunction can suffer from incontinence, pelvic pain, constipation, and voiding disturbance. These symptoms are signs of complex problems affecting the entire pelvic floor, so clinicians should treat the pelvic unit as a whole rather than isolated organs. For instance, pelvic muscle rehabilitation (PMR) manages pelvic floor dysfunction and associated symptoms. Pelvic floor physical therapy takes a